Brief notes and chronology of Western Medicine (1)
Beliefs in divine retribution are introduced, as are appeals to gods such as Mars and Carna for protection and healing. Readers are introduced to historiographical debates about demons and demonism in Late Antiquity. The Christian sanctification of sickness is discussed in depth, and compared with other theodicies of the ancient world. Distinctions between Christian and pagan philanthropy are also discussed. Medical training and education is examined in depth, with a marked focus on monasteries as centres of learning, universities in Europe, and the Alexandrian school in Egypt.
Distinctions between hospitals in the Latin West and the Byzantine Empire are also drawn. The link between divine and natural causation is clearly formulated: Various healers, including the prominent physician Avicenna, are discussed. The development of hospitals and Islamic medical ethics are briefly outlined. Historiographical debates about the nature of Islamic prophetic medicine are also covered. The argument that the Protestant Reformation precipitated shifts in the treatment of the sick poor is also covered. Indeed, the author points out that there were efforts to revive clerical medicine across Europe at the time.
The origins of nursing, asylums and medical missions are discussed in depth. Faith healing in pietistic circles in both European and American Protestantism is covered, as well as temperance movements associated with the influence of Methodism and Adventism. Biblical criticism, evolutionary theory and eugenics are explored. Discussions of Protestant and Catholic medical ethics, particularly in relation to birth control, abortion and euthanasia are analysed. New Age spirituality and CAM complimentary and alternative medicine are also outlined briefly.
As Ferngren notes, the qualified nurse Cicely Saunders — conceived of the movement following an evangelical conversion to Christianity. The volume closes with a provocative note on compassion. For Ferngren, compassion is a quality rooted in religious values, and lacks sustenance without a transcendent spiritual basis. Designed for the non-specialist, this book would be a good addition to student reading lists in a number of disciplines including history, theology and medicine. More generally, the work merits readership from any non-expert seeking a historical perspective on religious attitudes to sickness and healing.
Her title was "Lady Overseer of the Lady Physicians. The Atharvaveda , a sacred text of Hinduism dating from the Early Iron Age , is one of the first Indian text dealing with medicine. The Atharvaveda also contain prescriptions of herbs for various ailments. The use of herbs to treat ailments would later form a large part of Ayurveda.
Ayurveda, meaning the "complete knowledge for long life" is another medical system of India. Its two most famous texts belong to the schools of Charaka and Sushruta. The earliest foundations of Ayurveda were built on a synthesis of traditional herbal practices together with a massive addition of theoretical conceptualizations, new nosologies and new therapies dating from about BCE onwards, and coming out of the communities of thinkers who included the Buddha and others. Both these ancient compendia include details of the examination, diagnosis, treatment, and prognosis of numerous ailments.
Most remarkable is Sushruta's penchant for scientific classification: His medical treatise consists of chapters, 1, conditions are listed, including injuries and illnesses relating to aging and mental illness. The Ayurvedic classics mention eight branches of medicine: The teaching of various subjects was done during the instruction of relevant clinical subjects.
For example, teaching of anatomy was a part of the teaching of surgery, embryology was a part of training in pediatrics and obstetrics, and the knowledge of physiology and pathology was interwoven in the teaching of all the clinical disciplines. The normal length of the student's training appears to have been seven years. But the physician was to continue to learn. As an alternative form of medicine in India, Unani medicine got deep roots and royal patronage during medieval times.
It progressed during Indian sultanate and mughal periods. Unani medicine is very close to Ayurveda. Both are based on theory of the presence of the elements in Unani, they are considered to be fire, water, earth and air in the human body. According to followers of Unani medicine, these elements are present in different fluids and their balance leads to health and their imbalance leads to illness. By the 18th century CE, Sanskrit medical wisdom still dominated.
Muslim rulers built large hospitals in in Hyderabad , and in Delhi in , and numerous commentaries on ancient texts were written. China also developed a large body of traditional medicine. Much of the philosophy of traditional Chinese medicine derived from empirical observations of disease and illness by Taoist physicians and reflects the classical Chinese belief that individual human experiences express causative principles effective in the environment at all scales.
These causative principles, whether material, essential, or mystical, correlate as the expression of the natural order of the universe.
- Creole Son!
- The Reason of Things: Living with Philosophy!
- A brief history of Western culture?
- History of medicine?
The Jin Dynasty practitioner and advocate of acupuncture and moxibustion , Huangfu Mi — , also quotes the Yellow Emperor in his Jiayi jing , c. During the Tang Dynasty , the Suwen was expanded and revised, and is now the best extant representation of the foundational roots of traditional Chinese medicine. Traditional Chinese Medicine that is based on the use of herbal medicine, acupuncture, massage and other forms of therapy has been practiced in China for thousands of years.
In the 18th century, during the Qing dynasty, there was a proliferation of popular books as well as more advanced encyclopedias on traditional medicine. Jesuit missionaries introduced Western science and medicine to the royal court, the Chinese physicians ignored them. Because of the social custom that men and women should not be near to one another, the women of China were reluctant to be treated by male doctors. The missionaries sent women doctors such as Dr. Mary Hannah Fulton — Around BCE Homer in The Iliad gives descriptions of wound treatment by the two sons of Asklepios , the admirable physicians Podaleirius and Machaon and one acting doctor, Patroclus.
Because Machaon is wounded and Podaleirius is in combat Eurypylus asks Patroclus to cut out this arrow from my thigh, wash off the blood with warm water and spread soothing ointment on the wound. Temples dedicated to the healer-god Asclepius , known as Asclepieia Ancient Greek: Some of the surgical cures listed, such as the opening of an abdominal abscess or the removal of traumatic foreign material, are realistic enough to have taken place, but with the patient in a state of enkoimesis induced with the help of soporific substances such as opium.
He argued that channels linked the sensory organs to the brain, and it is possible that he discovered one type of channel, the optic nerves, by dissection. A towering figure in the history of medicine was the physician Hippocrates of Kos c. Most famously, the Hippocratics invented the Hippocratic Oath for physicians. Contemporary physicians swear an oath of office which includes aspects found in early editions of the Hippocratic Oath. Hippocrates and his followers were first to describe many diseases and medical conditions.
Though humorism humoralism as a medical system predates 5th-century Greek medicine, Hippocrates and his students systemetized the thinking that illness can be explained by an imbalance of blood, phlegm, black bile, and yellow bile. For this reason, clubbed fingers are sometimes referred to as "Hippocratic fingers". Shakespeare famously alludes to this description when writing of Falstaff 's death in Act II, Scene iii.
Hippocrates began to categorize illnesses as acute , chronic , endemic and epidemic , and use terms such as, "exacerbation, relapse , resolution, crisis, paroxysm , peak, and convalescence. Another of Hippocrates's major contributions may be found in his descriptions of the symptomatology, physical findings, surgical treatment and prognosis of thoracic empyema , i. His teachings remain relevant to present-day students of pulmonary medicine and surgery.
Hippocrates was the first documented person to practise cardiothoracic surgery , and his findings are still valid. Some of the techniques and theories developed by Hippocrates are now put into practice by the fields of Environmental and Integrative Medicine. These include recognizing the importance of taking a complete history which includes environmental exposures as well as foods eaten by the patient which might play a role in his or her illness. Two great Alexandrians laid the foundations for the scientific study of anatomy and physiology, Herophilus of Chalcedon and Erasistratus of Ceos.
Some of what we know of them comes from Celsus and Galen of Pergamum. Herophilus of Chalcedon , working at the medical school of Alexandria placed intelligence in the brain, and connected the nervous system to motion and sensation. Herophilus also distinguished between veins and arteries , noting that the latter pulse while the former do not.
He and his contemporary, Erasistratus of Chios , researched the role of veins and nerves , mapping their courses across the body. Erasistratus connected the increased complexity of the surface of the human brain compared to other animals to its superior intelligence. He sometimes employed experiments to further his research, at one time repeatedly weighing a caged bird, and noting its weight loss between feeding times.
In Erasistratus ' physiology, air enters the body, is then drawn by the lungs into the heart, where it is transformed into vital spirit, and is then pumped by the arteries throughout the body. Some of this vital spirit reaches the brain , where it is transformed into animal spirit, which is then distributed by the nerves. The Greek Galen c. He dissected animals to learn about the body, and performed many audacious operations—including brain and eye surgeries—that were not tried again for almost two millennia. In Ars medica "Arts of Medicine" , he explained mental properties in terms of specific mixtures of the bodily parts.
Galen's medical works were regarded as authoritative until well into the Middle Ages.
Navigation menu
Galen left a physiological model of the human body that became the mainstay of the medieval physician's university anatomy curriculum, but it suffered greatly from stasis and intellectual stagnation because some of Galen's ideas were incorrect; he did not dissect a human body. In the s Belgian anatomist and physician Andreas Vesalius launched a project to translate many of Galen's Greek texts into Latin.
Vesalius's most famous work, De humani corporis fabrica was greatly influenced by Galenic writing and form. The Romans invented numerous surgical instruments , including the first instruments unique to women, [57] as well as the surgical uses of forceps , scalpels , cautery , cross-bladed scissors , the surgical needle , the sound , and speculas. The Roman army physician Dioscorides c. He wrote the encyclopedia De Materia Medica describing over herbal cures, forming an influential pharmacopoeia which was used extensively for the following 1, years.
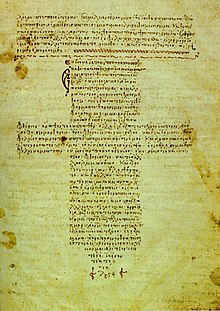
Byzantine medicine was notable for building upon the knowledge base developed by its Greco-Roman predecessors. In preserving medical practices from antiquity, Byzantine medicine influenced Islamic medicine as well as fostering the Western rebirth of medicine during the Renaissance. Byzantine physicians often compiled and standardized medical knowledge into textbooks. Their records tended to include both diagnostic explanations and technical drawings.
The Medical Compendium in Seven Books , written by the leading physician Paul of Aegina , survived as a particularly thorough source of medical knowledge. This compendium, written in the late seventh century, remained in use as a standard textbook for the following years. Late antiquity ushered in a revolution in medical science, and historical records often mention civilian hospitals although battlefield medicine and wartime triage were recorded well before Imperial Rome.
Constantinople stood out as a center of medicine during the Middle Ages, which was aided by its crossroads location, wealth, and accumulated knowledge. The first ever known example of separating conjoined twins occurred in the Byzantine Empire in the 10th century. The next example of separating conjoined twins will be first recorded many centuries later in Germany in The Byzantine Empire 's neighbors, the Persian Sassanid Empire , also made their noteworthy contributions mainly with the establishment of the Academy of Gondeshapur , which was "the most important medical center of the ancient world during the 6th and 7th centuries.
The Islamic civilization rose to primacy in medical science as its physicians contributed significantly to the field of medicine, including anatomy , ophthalmology , pharmacology , pharmacy , physiology , surgery , and the pharmaceutical sciences. The Arabs were influenced by ancient Indian, Persian, Greek, Roman and Byzantine medical practices, and helped them develop further. The translation of of Galen's works into Arabic by the Nestorian Christian Hunayn ibn Ishaq and his assistants, and in particular Galen's insistence on a rational systematic approach to medicine, set the template for Islamic medicine , which rapidly spread throughout the Arab Empire.
Its most famous physicians included the Persian polymaths Muhammad ibn Zakariya al-Razi and Avicenna , who wrote more than 40 works on health, medicine, and well-being.
Keep Exploring Britannica
Taking leads from Greece and Rome, Islamic scholars kept both the art and science of medicine alive and moving forward. Medical services were provided, especially for the poor, in the thousands of monastic hospitals that sprang up across Europe, but the care was rudimentary and mainly palliative. Isidore of Seville being the primary channel for transmitting Greek medical ideas.
Greek and Roman taboos had meant that dissection was usually banned in ancient times, but in the Middle Ages it changed: Wallis identifies a prestige hierarchy with university educated physicians on top, followed by learned surgeons; craft-trained surgeons; barber surgeons; itinerant specialists such as dentist and oculists; empirics; and midwives. The first medical schools were opened in the 9th century, most notably the Schola Medica Salernitana at Salerno in southern Italy. The cosmopolitan influences from Greek, Latin, Arabic, and Hebrew sources gave it an international reputation as the Hippocratic City.
Students from wealthy families came for three years of preliminary studies and five of medical studies. The medicine, following the laws of Federico II, that he founded in the University ad improved the Schola Salernitana, in the period between and , it had in Sicily so-called Sicilian Middle Ages a particular development so much to create a true school of Jewish medicine. As a result of which, after a legal examination, was conferred to a Jewish Sicilian woman, Virdimura, wife of another physician Pasquale of Catania, the hystorical record of before woman officially trained to exercise of the medical profession.
By the thirteenth century, the medical school at Montpellier began to eclipse the Salernitan school. In the 12th century, universities were founded in Italy, France, and England, which soon developed schools of medicine. Nearly all the learning was from lectures and readings in Hippocrates, Galen, Avicenna, and Aristotle.
Timeline of medicine and medical technology
The underlying principle of most medieval medicine was Galen's theory of humours. This was derived from the ancient medical works, and dominated all western medicine until the 19th century. The theory stated that within every individual there were four humours, or principal fluids—black bile, yellow bile, phlegm, and blood, these were produced by various organs in the body, and they had to be in balance for a person to remain healthy. Too much phlegm in the body, for example, caused lung problems; and the body tried to cough up the phlegm to restore a balance.
The balance of humours in humans could be achieved by diet, medicines, and by blood-letting , using leeches. The four humours were also associated with the four seasons, black bile-autumn, yellow bile-summer, phlegm-winter and blood-spring. Healing included both physical and spiritual therapeutics, such as the right herbs, a suitable diet, clean bedding, and the sense that care was always at hand.
Other procedures used to help patients included the Mass, prayers, relics of saints, and music used to calm a troubled mind or quickened pulse. In , in Sicily, it was historically given, in relationship to the laws of Federico II that they foresaw an examination with a regal errand of physicists, the first qualification to the exercise of the medicine to a woman, Virdimura a Jewess of Catania, whose document is preserved in Palermo to the Italian national archives.
The Renaissance brought an intense focus on scholarship to Christian Europe. A major effort to translate the Arabic and Greek scientific works into Latin emerged. Europeans gradually became experts not only in the ancient writings of the Romans and Greeks, but in the contemporary writings of Islamic scientists.
Ancient Greek medicine
During the later centuries of the Renaissance came an increase in experimental investigation, particularly in the field of dissection and body examination, thus advancing our knowledge of human anatomy. Vesalius described in detail the anatomy of the brain and other organs; he had little knowledge of the brain's function, thinking that it resided mainly in the ventricles.
Over his lifetime he corrected over of Galen 's mistakes. Understanding of medical sciences and diagnosis improved, but with little direct benefit to health care. Few effective drugs existed, beyond opium and quinine. Folklore cures and potentially poisonous metal-based compounds were popular treatments. Independently from Ibn al-Nafis , Michael Servetus rediscovered the pulmonary circulation , but this discovery did not reach the public because it was written down for the first time in the "Manuscript of Paris" [79] in , and later published in the theological work which he paid with his life in Later this was perfected by Renaldus Columbus and Andrea Cesalpino.
Later William Harvey correctly described the circulatory system. The most useful tomes in medicine used both by students and expert physicians were De Materia Medica and Pharmacopoeia.
Bacteria and protists were first observed with a microscope by Antonie van Leeuwenhoek in , initiating the scientific field of microbiology. Paracelsus — , was an erratic and abusive innovator who rejected Galen and bookish knowledge, calling for experimental research, with heavy doses of mysticism, alchemy and magic mixed in.
He rejected sacred magic miracles under Church auspisces and looked for cures in nature. His hermetical views were that sickness and health in the body relied on the harmony of man microcosm and Nature macrocosm. He took an approach different from those before him, using this analogy not in the manner of soul-purification but in the manner that humans must have certain balances of minerals in their bodies, and that certain illnesses of the body had chemical remedies that could cure them.
Paracelsus is a highly controversial figure in the history of medicine, with most experts hailing him as a Father of Modern Medicine for shaking off religious orthodoxy and inspiring many researchers; others say he was a mystic more than a scientist and downplay his importance. The University of Padua was founded about by walkouts from the University of Bologna , and began teaching medicine in It played a leading role in the identification and treatment of diseases and ailments, specializing in autopsies and the inner workings of the body.
- A White Wind Blew: A Novel.
- What is modern medicine??
- Towards a New Manifesto!
The intensive study of Galen led to critiques of Galen modeled on his own writing, as in the first book of Vesalius's De humani corporis fabrica. Andreas Vesalius held the chair of Surgery and Anatomy explicator chirurgiae and in published his anatomical discoveries in De Humani Corporis Fabrica. He portrayed the human body as an interdependent system of organ groupings. The book triggered great public interest in dissections and caused many other European cities to establish anatomical theatres. At the University of Bologna the training of physicians began in The Italian city attracted students from across Europe.
Taddeo Alderotti built a tradition of medical education that established the characteristic features of Italian learned medicine and was copied by medical schools elsewhere. He became Professor of Anatomy and Surgery at the University of Bologna in , where he established anatomy as a major branch of medicine for the first time.
Aranzi combined anatomy with a description of pathological processes, based largely on his own research, Galen, and the work of his contemporary Italians. Aranzi discovered the 'Nodules of Aranzio' in the semilunar valves of the heart and wrote the first description of the superior levator palpebral and the coracobrachialis muscles. His books in Latin covered surgical techniques for many conditions, including hydrocephalus , nasal polyp , goitre and tumours to phimosis , ascites , haemorrhoids , anal abscess and fistulae. Catholic women played large roles in health and healing in medieval and early modern Europe.
The Catholic elites provided hospital services because of their theology of salvation that good works were the route to heaven. The Protestant reformers rejected the notion that rich men could gain God's grace through good works—and thereby escape purgatory—by providing cash endowments to charitable institutions.
They also rejected the Catholic idea that the poor patients earned grace and salvation through their suffering. In London, the crown allowed two hospitals to continue their charitable work, under nonreligious control of city officials. They were employed by parishes and hospitals, as well as by private families, and provided nursing care as well as some medical, pharmaceutical, and surgical services. Meanwhile, in Catholic lands such as France, rich families continued to fund convents and monasteries, and enrolled their daughters as nuns who provided free health services to the poor.
Nursing was a religious role for the nurse, and there was little call for science. During the Age of Enlightenment , the 18th century, science was held in high esteem and physicians upgraded their social status by becoming more scientific. The health field was crowded with self-trained barber-surgeons, apothecaries, midwives, drug peddlers, and charlatans. Across Europe medical schools relied primarily on lectures and readings. The final year student would have limited clinical experience by trailing the professor through the wards.
Laboratory work was uncommon, and dissections were rarely done because of legal restrictions on cadavers. Most schools were small, and only Edinburgh, Scotland, with 11, alumni, produced large numbers of graduates. In Britain, there were but three small hospitals after Pelling and Webster estimate that in London in the to period, out of a population of nearly , people, there were about medical practitioners. Nurses and midwives are not included.
There were about 50 physicians, licensed surgeons, apothecaries, and additional unlicensed practitioners. The London Dispensary opened in , the first clinic in the British Empire to dispense medicines to poor sick people. The innovation was slow to catch on, but new dispensaries were open in the s. Guy's Hospital , the first great British hospital opened in in London, with funding from businessman Thomas Guy. Samuel Sharp —78 , a surgeon at Guy's Hospital, from to , was internationally famous; his A Treatise on the Operations of Surgery 1st ed.
English physician Thomas Percival — wrote a comprehensive system of medical conduct, Medical Ethics; or, a Code of Institutes and Precepts, Adapted to the Professional Conduct of Physicians and Surgeons that set the standard for many textbooks. In the Spanish Empire , the viceregal capital of Mexico City was a site of medical training for physicians and the creation of hospitals.
Aztec emperor Cuitlahuac died of smallpox. Medical education instituted at the Royal and Pontifical University of Mexico chiefly served the needs of urban elites. Male and female curanderos or lay practitioners, attended to the ills of the popular classes. The Spanish crown began regulating the medical profession just a few years after the conquest, setting up the Royal Tribunal of the Protomedicato, a board for licensing medical personnel in Licensing became more systematic after with physicians, druggists, surgeons, and bleeders requiring a license before they could publicly practice.
Elites and the popular classes alike called on divine intervention in personal and society-wide health crises, such as the epidemic of The intervention of the Virgin of Guadalupe was depicted in a scene of dead and dying Indians, with elites on their knees praying for her aid. In the late eighteenth century, the crown began implementing secularizing policies on the Iberian peninsula and its overseas empire to control disease more systematically and scientifically.
The practice of medicine changed in the face of rapid advances in science, as well as new approaches by physicians. Hospital doctors began much more systematic analysis of patients' symptoms in diagnosis. However the decline in many of the most lethal diseases was due more to improvements in public health and nutrition than to advances in medicine. Medicine was revolutionized in the 19th century and beyond by advances in chemistry, laboratory techniques, and equipment.
Old ideas of infectious disease epidemiology were gradually replaced by advances in bacteriology and virology. In the s in Italy, Agostino Bassi traced the silkworm disease muscardine to microorganisms. Meanwhile, in Germany, Theodor Schwann led research on alcoholic fermentation by yeast , proposing that living microorganisms were responsible. Leading chemists, such as Justus von Liebig , seeking solely physicochemical explanations, derided this claim and alleged that Schwann was regressing to vitalism.
In in Vienna, Ignaz Semmelweis — , dramatically reduced the death rate of new mothers due to childbed fever by requiring physicians to clean their hands before attending childbirth , yet his principles were marginalized and attacked by professional peers. Eminent French scientist Louis Pasteur confirmed Schwann 's fermentation experiments in and afterwards supported the hypothesis that yeast were microorganisms. Moreover, he suggested that such a process might also explain contagious disease. In , Pasteur's report on bacterial fermentation of butyric acid motivated fellow Frenchman Casimir Davaine to identify a similar species which he called bacteridia as the pathogen of the deadly disease anthrax.
Others dismissed "bacteridia" as a mere byproduct of the disease. British surgeon Joseph Lister , however, took these findings seriously and subsequently introduced antisepsis to wound treatment in German physician Robert Koch , noting fellow German Ferdinand Cohn 's report of a spore stage of a certain bacterial species, traced the life cycle of Davaine 's bacteridia , identified spores, inoculated laboratory animals with them, and reproduced anthrax—a breakthrough for experimental pathology and germ theory of disease. Pasteur's group added ecological investigations confirming spores' role in the natural setting, while Koch published a landmark treatise in on the bacterial pathology of wounds.
In , Koch reported discovery of the " tubercle bacillus ", cementing germ theory and Koch's acclaim. Upon the outbreak of a cholera epidemic in Alexandria, Egypt , two medical missions went to investigate and attend the sick, one was sent out by Pasteur and the other led by Koch. On losing the rivalry in Alexandria, Pasteur switched research direction, and introduced his third vaccine— rabies vaccine —the first vaccine for humans since Jenner 's for smallpox.
Although his proposed tuberculosis treatment, tuberculin , seemingly failed, it soon was used to test for infection with the involved species. In , Koch was awarded the Nobel Prize in Physiology or Medicine , and remains renowned as the founder of medical microbiology. Women had always served in ancillary roles, and as midwives and healers. The professionalization of medicine forced them increasingly to the sidelines. As hospitals multiplied they relied in Europe on orders of Roman Catholic nun-nurses, and German Protestant and Anglican deaconesses in the early 19th century.
They were trained in traditional methods of physical care that involved little knowledge of medicine. The breakthrough to professionalization based on knowledge of advanced medicine was led by Florence Nightingale in England. She resolved to provide more advanced training than she saw on the Continent. At Kaiserswerth, where the first German nursing schools were founded in by Theodor Fliedner , she said, "The nursing was nil and the hygiene horrible.
The Nightingale solution depended on the patronage of upper class women, and they proved eager to serve. In the wife of the British king took control of the nursing unit of the British army, became its president, and renamed it after herself as the Queen Alexandra's Royal Army Nursing Corps ; when she died the next queen became president. In the United States, upper middle class women who already supported hospitals promoted nursing. The new profession proved highly attractive to women of all backgrounds, and schools of nursing opened in the late 19th century.
They soon a function of large hospitals, where they provided a steady stream of low-paid idealistic workers. The International Red Cross began operations in numerous countries in the late 19th century, promoting nursing as an ideal profession for middle class women. The Nightingale model was widely copied. Linda Richards — studied in London and became the first professionally trained American nurse.
She established nursing training programs in the United States and Japan, and created the first system for keeping individual medical records for hospitalized patients. They ran hospitals, clinics, almshouses, pharmacies, and shelters as well as training schools for nurses. In the Soviet era — , with the aristocratic sponsors gone, nursing became a low-prestige occupation based in poorly maintained hospitals.
It was very difficult for women to become doctors in any field before the s. Elizabeth Blackwell — became the first woman to formally study and practice medicine in the United States. She was a leader in women's medical education. While Blackwell viewed medicine as a means for social and moral reform, her student Mary Putnam Jacobi — focused on curing disease. At a deeper level of disagreement, Blackwell felt that women would succeed in medicine because of their humane female values, but Jacobi believed that women should participate as the equals of men in all medical specialties using identical methods, values and insights.
Paris France and Vienna were the two leading medical centers on the Continent in the era — In the s—s Paris became a world center of medical research and teaching. The "Paris School" emphasized that teaching and research should be based in large hospitals and promoted the professionalization of the medical profession and the emphasis on sanitation and public health. He created the Paris Hospital, health councils, and other bodies.
Louis Pasteur — was one of the most important founders of medical microbiology. He is remembered for his remarkable breakthroughs in the causes and preventions of diseases. His discoveries reduced mortality from puerperal fever , and he created the first vaccines for rabies and anthrax. His experiments supported the germ theory of disease. He was best known to the general public for inventing a method to treat milk and wine in order to prevent it from causing sickness, a process that came to be called pasteurization.
He is regarded as one of the three main founders of microbiology , together with Ferdinand Cohn and Robert Koch. He worked chiefly in Paris and in founded the Pasteur Institute there to perpetuate his commitment to basic research and its practical applications. As soon as his institute was created, Pasteur brought together scientists with various specialties.
The first five departments were directed by Emile Duclaux general microbiology research and Charles Chamberland microbe research applied to hygiene , as well as a biologist, Ilya Ilyich Mechnikov morphological microbe research and two physicians , Jacques-Joseph Grancher rabies and Emile Roux technical microbe research. One year after the inauguration of the Institut Pasteur, Roux set up the first course of microbiology ever taught in the world, then entitled Cours de Microbie Technique Course of microbe research techniques. It became the model for numerous research centers around the world named "Pasteur Institutes.
The First Viennese School of Medicine, —, was led by the Dutchman Gerard van Swieten — , who aimed to put medicine on new scientific foundations—promoting unprejudiced clinical observation, botanical and chemical research, and introducing simple but powerful remedies. When the Vienna General Hospital opened in , it at once became the world's largest hospital and physicians acquired a facility that gradually developed into the most important research centre.
Vienna was the capital of a diverse empire and attracted not just Germans but Czechs, Hungarians, Jews, Poles and others to its world-class medical facilities. Basic medical science expanded and specialization advanced. Furthermore, the first dermatology , eye, as well as ear, nose, and throat clinics in the world were founded in Vienna. The textbook of ophthalmologist Georg Joseph Beer — Lehre von den Augenkrankheiten combined practical research and philosophical speculations, and became the standard reference work for decades.
A Brief History of Medicine
After Berlin, the capital of the new German Empire, became a leading center for medical research. Robert Koch — was a representative leader. He became famous for isolating Bacillus anthracis , the Tuberculosis bacillus and Vibrio cholerae and for his development of Koch's postulates. He was awarded the Nobel Prize in Physiology or Medicine in for his tuberculosis findings.
Koch is one of the founders of microbiology , inspiring such major figures as Paul Ehrlich and Gerhard Domagk. In the American Civil War —65 , as was typical of the 19th century, more soldiers died of disease than in battle, and even larger numbers were temporarily incapacitated by wounds, disease and accidents. Weapon development -particularly the appearance of Springfield Model , mass-produced and much more accurate than muskets led to generals underestimating the risks of long range rifle fire; risks exemplified in the death of John Sedgwick and the disastrous Pickett's Charge.
The rifles could shatter bone forcing amputation and longer ranges meant casualties were sometimes not quickly found. Evacuation of the wounded from Second Battle of Bull Run took a week. The hygiene of the training and field camps was poor, especially at the beginning of the war when men who had seldom been far from home were brought together for training with thousands of strangers.
First came epidemics of the childhood diseases of chicken pox, mumps, whooping cough, and, especially, measles. Operations in the South meant a dangerous and new disease environment, bringing diarrhea, dysentery, typhoid fever, and malaria. There were no antibiotics, so the surgeons prescribed coffee, whiskey, and quinine. Harsh weather, bad water, inadequate shelter in winter quarters, poor policing of camps, and dirty camp hospitals took their toll.
This was a common scenario in wars from time immemorial, and conditions faced by the Confederate army were even worse. The Union responded by building army hospitals in every state. What was different in the Union was the emergence of skilled, well-funded medical organizers who took proactive action, especially in the much enlarged United States Army Medical Department, [] and the United States Sanitary Commission , a new private agency.
A major breakthrough in epidemiology came with the introduction of statistical maps and graphs. They allowed careful analysis of seasonality issues in disease incidents, and the maps allowed public health officials to identify critical loci for the dissemination of disease. John Snow in London developed the methods. In , he observed that the symptoms of cholera, which had already claimed around lives within a month, were vomiting and diarrhoea. He concluded that the source of contamination must be through ingestion, rather than inhalation as was previously thought.
It was this insight that resulted in the removal of The Pump On Broad Street, after which deaths from cholera plummeted afterwards. English nurse Florence Nightingale pioneered analysis of large amounts of statistical data, using graphs and tables, regarding the condition of thousands of patients in the Crimean War to evaluate the efficacy of hospital services. Her methods proved convincing and led to reforms in military and civilian hospitals, usually with the full support of the government.
By the late 19th and early 20th century English statisticians led by Francis Galton , Karl Pearson and Ronald Fisher developed the mathematical tools such as correlations and hypothesis tests that made possible much more sophisticated analysis of statistical data. Civil War the Sanitary Commission collected enormous amounts of statistical data, and opened up the problems of storing information for fast access and mechanically searching for data patterns. The pioneer was John Shaw Billings — A senior surgeon in the war, Billings built the Library of the Surgeon General's Office now the National Library of Medicine , the centerpiece of modern medical information systems.
The applications were developed by his assistant Herman Hollerith ; Hollerith invented the punch card and counter-sorter system that dominated statistical data manipulation until the s. Johns Hopkins Hospital , founded in , originated several modern medical practices, including residency and rounds. European ideas of modern medicine were spread widely through the world by medical missionaries, and the dissemination of textbooks.
Japanese elites enthusiastically embraced Western medicine after the Meiji Restoration of the s. However they had been prepared by their knowledge of the Dutch and German medicine, for they had some contact with Europe through the Dutch.
